
AHA BLS For Healthcare Providers Initial Provider Certification at First In Last Out Medical Response 3322 Coors Blvd NW Suite 4 Albuquerque, NM 87120
American Heart Association AHA
FIRST IN LAST OUT MEDICAL RESPONSE CERTIFICATIONS 3322 COORS BLVD NW SUITE 4 ALBUQUERQUE, NM 87120 GERARDO REYES (505) 358-1197
American Heart Association BLS Basic Life Support for Healthcare Providers Renewal courses at First In Last Out Medical Response 3322 Coors Blvd NW Suite 4 Albuquerque, NM 87120.
Are you paying more than $50 for your BLS class? We have NO HIDDEN FEES! Cost includes E-Book, certification card and tax!
Please be sure to download all the documents required for class. There is an agenda, skills check off sheets and your E-book, Algorithms and more!
The AHA Basic Life Support (BLS) for Healthcare Providers Renewal Course is the refresher version of the BLS Initial course designed for healthcare providers who already possess a valid (or recently expired) AHA BLS certification. Its goal is to refresh, validate, and extend the BLS skills and knowledge so the provider can continue to respond to cardiopulmonary emergencies.
Here’s a breakdown of what that renewal course generally involves:
This course is intended for healthcare professionals (nurses, physicians, EMTs/paramedics, respiratory therapists, etc.) who already hold a valid AHA BLS Provider card (or one that’s just expired, typically within a grace period).
It is not an “initial” course — it doesn’t teach everything from scratch, but rather reviews and reassesses core BLS skills and critical concepts.
In the renewal course, participants typically review and perform:
High-quality CPR for adults, children, and infants (single rescuer and team-based)
Use of an AED (automated external defibrillator)
Ventilations / rescue breathing techniques (using barrier devices, bag-mask ventilation)
Relief of foreign-body airway obstruction (choking) in both conscious and unconscious victims (adult, child, infant)
Team dynamics and coordination in multi-rescuer settings
Review of the AHA Chain of Survival (emphasis on early recognition, CPR, defibrillation)
For some courses: introduction or review of CPR with an advanced airway (if relevant)
The BLS Renewal class as covering adult/child/infant CPR (including two-rescuer), bag-mask ventilation, foreign body airway obstruction, and AED use. showmecpr.com
The renewal class is usually instructor-led (classroom / hands-on). Some centers might incorporate blended elements, but renewal courses tend to be more focused on skills practice.
The duration is shorter than an initial BLS course (since less new content is taught). Many renewal sessions are 2 to 3 hours or less. showmecpr.com
Participants must successfully complete hands-on skill stations where instructors observe and evaluate their performance (e.g. compressions, ventilations, AED use, choking relief).
A written or knowledge test is often part of the renewal process
On passing both the psychomotor (skills) and cognitive assessments, participants receive a BLS Provider Course Completion Card (or eCard) that's valid for another 2 years. cpr.heart.org
Basic Life Support is a life saving certification class that teaches how to perform CPR or Cardiopulmonary Resuscitation by providing chest compressions combined with rescue breaths. It also teaches how to use an AED or automatic external defibrillator and a bag mask device. Training is provided for Adults, Child and infants. Choking is included in the course.
Basic Life Support is the foundation for saving lives after cardiac arrest. You will learn the skills of high-quality cardiopulmonary resuscitation (CPR) for victims of all ages and will practice delivery of these skills both as a single rescuer and as a member of a multi-rescuer team. The skills you learn in this course will enable you to recognize cardiac arrest, activate the emergency response system early, and respond quickly and confidently.
Despite important advances in prevention, sudden cardiac arrest remains a leading cause of death in the Unites States. Seventy percent of out-of-hospital cardiac arrests occur in the home. About half are unwitnessed. Outcome from out-of-hospital cardiac arrest remains poor. Only about 10% of adult patients with non-traumatic cardiac arrest who are treated by emergency medical services (EMS) survive to hospital discharge.
With the knowledge and skills you learn in this course, your actions can give victims the best chance of survival.
The BLS Course focuses on what rescuers need to know to perform high-quality CPR in a wide variety of settings. You will also learn how to respond to choking emergencies.
After successfully completing the BLS Course, you should be able to
*Describe the importance of high-quality CPR and its impact on survival
*Describe all of the steps of the Chain of Survival
*Apply the BLS Concepts of the Chain of Survival
*Recognize the signs of someone needing CPR
*Perform high-quality CPR for an adult
* Describe the importance of early use of an AED
*Demonstrate the appropriate use of an AED
*Provide effective ventilations by using a barrier device
*Perform high quality CPR for a child
*Perform high quality CPR for an infant
*Describe the importance of teams in multi-rescuer resuscitation
*Perform as an effective team member during multi-rescuer CPR
*Describe the technique for relief of foreign-body airway obstruction for an adult or child
*Describe the technique for relief of foreign-body airway obstruction for an infant
This is the most expensive way to get certified. The online course is $38 and the in person portion is $50. It's cheaper to just come to class. Renewal is three hours and Initial is 4-5 and the total cost is $50. Includes tax, certification card and your e-book!
During the skills session a BLS instructor will guide the student through a series of scenarios consisting of adult, child and infant CPR using a bag mask device and an AED.
Basic Life Support (BLS) skills testing is a live exam that assesses a student's ability to perform BLS skills they learned during certification. The test is designed to evaluate a student's knowledge and proficiency in performing essential BLS skills, such as chest compressions, rescue breathing, and automated external defibrillation (AED).
You will first practice and then be tested on 1 Rescuer Adult CPR with a bag mask and then 2 Rescuer Adult CPR with a bag mask and an AED.
Next you will practice and then be tested on 1 and 2 rescuer infant CPR with a bag mask, pocket mask and AED.
Upon successful completion of the course, students will receive a same day American Heart Association 2025 Guidelines BLS Provider Card valid for two years.
A Basic Life Support (BLS) Skills Checkoff is a hands-on evaluation by a certified instructor, verifying a learner's competence in life-saving techniques like high-quality CPR (compressions & breaths), AED use, and team dynamics for adults, children, and infants, often after completing online training, to get an official BLS certification card. It assesses critical steps, including scene safety, responsiveness checks, calling for help, proper hand placement, compression rate/depth, chest recoil, and effective rescue breaths, ensuring readiness for real emergencies.
This is the most expensive way to get certified. The online course is $38 and the in person portion is $50. It's cheaper to just come to class. Renewal is three hours and Initial is 4-5 and the total cost is $50. Includes tax, certification card and your e-book!
Please be sure to download all the documents required for class. There is an agenda, skills check off sheets and your E-book, Algorithms and more!
An AHA Basic Life Support (BLS) in-person skills checkoff (sometimes called the “skills session” or “skills check-off”) is the hands-on, instructor-led component during which students demonstrate their practical BLS (CPR / AED / choking) skills under observation. It is required to complete a full BLS certification or renewal if the didactic/online portion has already been completed (e.g., in a blended-learning or HeartCode format).
Here’s what it involves, what’s expected, and how it fits into the course:
The skills checkoff is solely focused on psychomotor skills (doing, not just knowing). It ensures that learners can correctly perform BLS techniques (compressions, ventilations, AED use, choking relief) per the AHA’s current guidelines.
It verifies that participants meet the performance criteria necessary for patient safety—i.e., quality and accuracy, not just theory.
For blended (HeartCode® BLS) or “online + hands-on” BLS courses, this is the in-person final step after completing the online didactic portion. cpr.heart.org
During the checkoff, participants must perform various BLS skills according to the AHA rubric. Typical elements include:
| Skill | What You Must Demonstrate |
|---|---|
| High-quality CPR (Adult, Child, Infant) | Proper hand placement, correct rate & depth, full chest recoil, minimal interruptions |
| Ventilations / Rescue Breaths | Use of barrier device (pocket mask, face shield) or bag–mask ventilation with adequate tidal volume, correct timing |
| AED / Defibrillator Use | Power on/off, pad placement, “clear” before shock, safe shock delivery, resume compressions immediately |
| Choking / Foreign-Body Airway Obstruction Relief | Techniques for conscious and unconscious victims (adult, child, infant) |
| Team / Multi-rescuer Coordination | In scenarios with more than one rescuer, demonstrating role clarity, communication, smooth transitions, etc. |
The performance is usually evaluated with a step-by-step checklist where each required action must be correctly and confidently performed.
If any key step is missed, the instructor may require remediation and retesting until standards are met.
The skills checkoff usually takes 60 to 120 minutes (or sometimes less, depending on facility & number of students). cpr.heart.org+1
Participants are scheduled for a hands-on session (often in a classroom, skills lab, or training center) with manikins, AED training units, and airway equipment.
In many centers, the checkoff is done after (or following) the online/cognitive portion has been completed. For example, for HeartCode® BLS, you complete the online portion first, then attend the in-person skills session. cpr.heart.org
Some training centers offer “skills-only” sessions (also called “BLS Provider Skills Check Only”) for students who have already completed the knowledge/online part but still need to validate their hands-on skills. cprcertifiedtrainer.com
Participants must pass the skills checkoff (i.e., meet all the required steps) to be awarded the BLS Provider Course Completion Card (or eCard), valid for two years. CPR Training School+3cpr.heart.org+3cpr.heart.org+3
If a participant fails to perform any required skill adequately, remediation is given and the learner may repeat that portion or the entire checkoff until they meet the standard.
Once the hands-on portion is passed (or skills checkoff is successfully completed), combined with completion of any cognitive/online portion, the course is considered fulfilled and certification is granted.
2025 Guidelines Changes – Released October 22, 2025
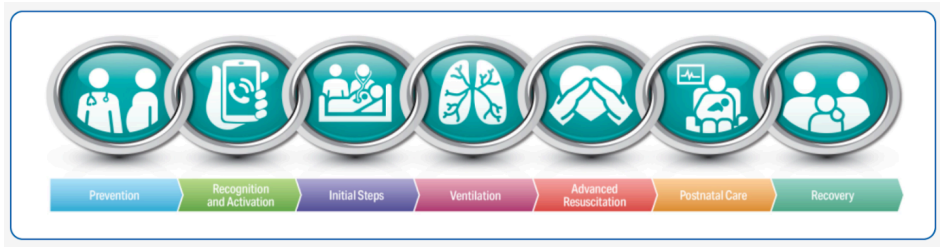
New Chain of Survival This single chain applies to adult and pediatric in-hospital cardiac arrest and out of
hospital cardiac arrest.

Newborn Chain of Survival
New update to Adult BLS Algorithm to include the role of opioid antagonists for
suspected opioid overdose during respiratory and cardiac arrest.
Toxicology: Opioid Overdose
For lay and trained rescuers, administering an opioid antagonist for adults and
children provided it does not interfere with High Quality CPR and breaths.
Adults and Children treated for opioid overdose are at high risk of subsequent
overdoses. They should receive psychosocial interventions, referral to treatments
programs and take home opioid antagonists and instructions on how to use them.
Foreign-Body Airway Obstruction: Adults, Children and Infants
New 2025: For adults with severe foreign-body airway obstruction (FBAO),
repeated cycles of back blows followed by 5 abdominal thrusts should be
performed until the object is expelled or the person becomes unresponsive.
With infants (under one year) when performing chest thrusts, use the palm of
one hand, or encircle the infants chest and compress with two thumbs.
AED Pad Placement
Anterolateral (High right, low left) or Anteroposterior (AP) Placement - 2
options
1). Center of the chest and center of the back
2) Place one on the upper left chest above the nipple and the other on the left
side of the back near the spine
It is reasonable to adjust the position of a patient's bra instead of removing it
when placing pads
HEAD AND NECK INJURY
When head and neck injury are present, lay rescuers should maintain manual
spinal motion restriction and should not use rigid cervical collar devices.
Spinal immobilization devices such as rigid cervical collars may make it more
difficult to maintain airway patency and provide adequate ventilation.
Maintaining a patent airway and providing adequate ventilation and
oxygenation are priorities during CPR. If a jaw thrust and insertion of an
airway adjunct are ineffective, a head tilt–chin lift may be necessary to open
the airway. The importance of a patent airway outweighs the risk of further
spinal damage in the cardiac arrest patient even in the setting of head and
neck trauma.
Special Circumstances – Ventilation
Mouth-to-nose ventilation may be necessary if ventilation through the
person’s mouth is impossible because of trauma, positioning, or difficulty
obtaining a seal.
Changes in Adult Cardiac Arrest Algorithm
After identifying an adult in cardiac arrest, a lone responder should activate
the emergency response system first, then immediately begin CPR.
In adult cardiac arrest, rescuers should perform chest compressions with the
patient’s torso at approximately the level of the rescuer’s knees.
CPR for adult cardiac arrest patients with obesity should be provided by using
the same techniques as for the average weight patient.
Alternatives to conventional CPR Mechanical CPR devices may be used in special circumstances where the rescuer is not lateral to the patient.
One alternative position has been termed “over-the-head” compressions may
be provided with or without ventilations.
The rescuer may use their heel or foot to perform compressions when
patients are in unusual locations or when resuscitation must take place under
special circumstances.
Here is the continued information for the class. These things have stayed the
same and did not change with the New 2025 guidelines.
WHEN YOU FIND AN UNCONSCIOUS ADULT
STEP 1: Assess scene safety. Always assess scene safety first. If the scene is not
safe, it is reasonable to withhold resuscitation efforts.
STEP 2: Tap on both shoulders and shout "Hey are you ok?"
STEP 3: Activate the Emergency Response System and get an AED. If others
are around, send someone to get help.
Step 4: If you are a lone rescuer you should activate the emergency response
system first, then immediately begin CPR.
STEP 5: Assess breathing and pulse simultaneously: Check a carotid pulse for
at least 5 seconds but no more than 10. If there is no pulse or you are not sure
if you feel a pulse, begin chest compressions.
Compress at a depth of at least 2 inches or 5 cm for adults and children but
no more than 2.4 inches or 6 cm
Compress at a rate of at least 100-120 compressions per minute. Push hard
and fast. Make sure you allow the chest to completely recoil between
compressions.
After 30 compressions, give 2 breaths. If there is no suspected head or neck
injury: Perform a "head tilt chin lift" and give 2 breaths.
If you suspect a neck
injury: Perform a "jaw thrust" to open the airway and deliver 2 breaths.
Give each breath over 1 second watching for chest rise. Do not give large
breaths. You want to see the chest just begin to rise. If you give breaths that
are too large or too fast, all that extra air will go into the stomach. After several
large breaths, the pressure will begin to increase in stomach which will then
crush the lungs, heart and the diaphragm making it more difficult to save
your patient and they will most likely vomit.
Give cycles of 30 compressions and 2 breaths. 5 cycles = two minutes
STEP 6: After 2 minutes, reassess the pulse. If there is no pulse, resume chest
compressions and breaths for 2 more minutes. Every two minutes check a
pulse.
If you are not alone, switch roles every two minutes. The person giving
compressions will now maintain the airway and give breaths. The person who
was giving breaths will now take over chest compressions.
IF THEY HAVE A PULSE – Give one breath every 6 seconds. After every two
minutes, check for a pulse again. If there is no pulse begin CPR. If they have a
pulse and are still not breathing effectively, continue one breath every 6
seconds and check for a pulse every 2 minutes.
ONCE THE AED ARRIVES
When an AED arrives, use it.
Step 1: Turn on the AED. It may take up to 5-15 seconds to warm up.
8
Step 2: Follow the instructions given by the AED.
STEP 3: Place the pads on the patient following the pictures on the pads for
correct placement. If you are not alone, continue chest compressions and
have someone else place the pads. If the chest is hairy, the pads may not
stick, if you have 2 sets of pads, put them on the patient and pull them off
quickly to remove the hair. If you only have one set of pads, look in your AED
kit for a razor, scissors, and quickly remove some of the hair, and replace the
pads.
STEP 4: When the AED says "ANALYZING RHYTHM, DO NOT TOUCH THE
PATIENT" make sure no one is touching the patient, not even the person
giving breaths. If the AED says "SHOCK ADVISED, CHARGING" continue chest
compressions while the AED is charging.
STEP 5: When the AED is charged, clear the patient and deliver the shock.
Immediately resume chest compressions. Begin with 30 compressions and 2
breaths. Complete 5 cycles of 30 compressions and 2 breaths. When 2
minutes have passed, the AED will automatically reanalyze the rhythm.
If the AED says: "NO SHOCK ADVISED" you do not check a pulse, you
immediately resume CPR for 2 more minutes. Continue these steps until
more advanced help arrives.
Every time the AED reanalyzes the rhythm, the person giving compressions
should trade places with the person giving breaths. This is very important,
even if you are not tired. Your first several compressions are good and strong
but as time passes, you will begin to get tired and your compressions will be
less effective, even if you don't feel yourself getting tired. You need a two
minute rest so that you can begin again nice and fresh.
Always assess scene safety first. If the scene is not safe, it is reasonable to
withhold resuscitation efforts. If you find someone unconscious in the middle
of the street and run out to save them and get hit by a car, the situation just
got worse and now there are two people needing to be saved.
The American Heart Association still recommends the C-A-B sequence. When
a cardiac arrest happens, there is usually enough oxygen in the blood stream
to sustain life, but it must circulate throughout the body. So the most
important step to begin with is chest compressions, not rescue breaths.
Beginning with chest compressions is the easiest step for bystanders to
perform. It will only delay rescue breaths by about 18 seconds.
An AED only detects 2 particular heart rhythms. They are Ventricular
Fibrillation or V-Fib and Pulseless Ventricular Tachycardia or Pulseless V-Tach.
If the AED detects either of these rhythms it will deliver a shock.
The biggest misconception people have is that when you shock someone,
you jump start the heart just like you would jump start a car. This is not true.
When the heart is in Ventricular Fibrillation or Pulseless Ventricular
Tachycardia the heart is quivering. The heart is getting told to contract too
fast, from too many different cells that it can't possibly keep up and just
begins to vibrate. Almost like seeing someone on TV having a seizure. The
heart just vibrates. The only way to correct all the overstimulation is to stop all
of the electricity in the heart. For example: My computer gets a virus. The first
thing I want to do is pull the cord from the wall and stop the virus. I don't
want to start opening other programs and get them running too. The same
goes for V-Fib and Pulseless V-Tach.
The shock stops the heart completely, giving it a chance to start over and
hopefully produce a normal organized rhythm. So if defibrillating actually
stops the heart, do you see why shocking someone in asystole doesn't make
any sense? Why shock someone to stop the heart, when their heart is already
stopped.
Always allow the chest to completely recoil when doing compressions. Say
there was a small fire, and you had a water bottle full of water. Would it make
sense to squeeze tiny amounts out really fast; or, would it make more sense to
give the bottle a good squeeze and force out as much water as you can at one
time, and repeat? When you compress the chest, it squeezes a small amount
of blood out; by letting the chest completely recoil with each compression,
more blood is squeezed out with every compression.
RESCUE BREATHING:
For an adult, give 1 breath every 6 seconds.
For a child/infant, give 1 breath every 2 to 3 seconds or 20 to 30 breaths per
min. Children run faster than adults, so they must breathe faster too.
If an advanced airway (ETT) is in place regardless of age deliver one breath
every 6 seconds. If someone has an advanced airway in place, they will not be
conscious. If the person is "sleeping" they will not need to breathe as fast as
an adult or child and is the slowest rate of all. Only 1 breath every 6 seconds.
This is only 10 breaths per minute. When an advanced airway is used,
compressions must be stopped until the tube in placed in the airway. Once it
is in place, provide continuous chest compressions without pauses for the
breaths. (The tubes are very stiff and firm, slightly flexible. But they are firm
enough and long enough to allow oxygen to pass through them effectively
while someone is pushing down and compressing the chest.
Cardiac Arrest in Pregnancy
Do not delay providing chest compressions for a pregnant woman in cardiac
arrest. High-quality CPR can increase the mother’s and the infant’s chance of
survival. If you do not perform CPR on a pregnant woman when needed, the
lives of both the mother and the infant are at risk.
Perform high-quality chest compressions for a pregnant woman in cardiac
arrest as you would for any victim of cardiac arrest, but if a second rescuer is
available and the abdomen is visibly rounded, have the second rescuer hold
the abdomen on the mothers left side (to improve circulation).
Use an AED for a pregnant woman in cardiac arrest as you would for any
victim of cardiac arrest. If the woman begins to move, speak, blink, or
otherwise react, stop CPR and roll her onto her left side.
Debriefing for Rescuers
Debriefings and referral for follow-up for emotional support for lay rescuers,
EMS providers, and hospital-based healthcare workers after a cardiac arrest
event may be beneficial.
Rescuers may experience anxiety or post-traumatic stress about providing or
not providing basic life support. Hospital-based care providers may also
experience emotional or psychological effects of caring for a patient with
cardiac arrest. Team debriefings may allow a review of team performance
(education, quality improvement), as well as recognition of the natural
stressors associated with caring for a patient near death.
CHILD SPECIFIC
A CHILD is considered to be 1 year old, up to puberty. (Not an age, but physical
signs of puberty)
For lone rescuers, to provide child CPR, use one hand instead of two and
compress 2 inches = 5 cm (The same as an adult) or compress 1/3 the depth
of the chest. Deliver 30 compressions and 2 breaths.
When there are TWO RESCUERS, and the child is UNDER PUBERTY the
compression to ventilation ratio changes to 15:2 (Now, 10 cycles is 2 minutes
- Check the pulse every two minutes)
ONE MORE VERY IMPORTANT THING ABOUT PEDIATRIC PATIENTS
(CHILDREN & INFANTS)
If the child or infant (UNDER PUBERTY) HAS A PULSE OF 60 or less WITH
signs of poor perfusion or signs of cyanosis BEGIN CHEST COMPRESSIONS.
Only perform chest compressions if they also show signs of poor perfusion.
Only perform chest compressions if they also show signs of cyanosis (turning
blue because they are not getting enough oxygen, It is usually around the
mouth, lips and even fingertips.
Are they blue / cold are their fingers or lips blue, does their color just not look
right? Are there any signs the child is not getting enough blood supply and
oxygen?)
BEGIN CHEST COMPRESSIONS. DO NOT DELAY.
MAJOR DIFFERENCES IN CHILD AND ADULT CPR:
Over puberty is treated as an adult. Puberty is not defined by age, but instead
by physical appearance.
For boys: If there is any chest hair, or underarm hair present, they are
considered an adult. You cannot use facial hair (either beard or mustache or
"peach fuzz") to determine puberty. Some little boys sneak in the bathroom
and shave their face like daddy, and they get facial hair before puberty.)
For girls: Look for signs of breast development. If any breast development is
present they are considered an adult. So, if you had a 10 year old girl who
happens to be pregnant, she has hit puberty and is treated as an adult.
An INFANT is from birth to 1 year old.
For 2 rescuers, to provide infant CPR, wrap both hands around the infant's
chest and place both thumbs on the lower half of the breastbone. If the infant
is very little, you may need to place one of your thumbs on top of the other.
You can also use the palm of one hand.
Compress 1 1/2 inches = 4 cm or 1/3 the depth of the chest.
2 Rescuers deliver 15 compressions and 2 breaths.
ALONE - give 30 compressions and 2 breaths.
DIFFERENCES WITH AN AED USED ON CHILDREN AND INFANTS
Some AEDs have Adult and Pediatric pads. Pediatric pads should be used on
anyone 8 yrs and under. If pediatric pads are not available you should use the
adult pads on an infant or child. For a child, follow the pictures on the pads for
proper placement, making sure they do not touch, or overlap.
For an infant, place one pad in the center of the chest, and one pad on the
back in the center. If you can, remember "baby sandwich". Pads used on
infants under 1 year old are always placed front and back whether you are
using pediatric or adult pads.
Adult pads can be used on an infant under 1 year old if you only have adult
pads. A burned baby is better than a dead baby, and if a shock is needed it
must be delivered.
Never cut the adult pads in half. This will leave a bare metal edge which will
allow the shock to arc and shock someone else.
WHEN TO CALL FOR HELP AND WHEN TO START COMPRESSIONS
If an adult, check responsiveness, tap and shout "Hey, are you ok ?"
Check for breathing: if no breathing activate emergency response system
and get an AED Check for a pulse: if no pulse begin chest compressions at a
rate of 30:2 For an adult, the compression to ventilation ratio is always 30:2
with 1 or 2 rescuers.
If the victim is UNDER PUBERTY, and there are 2 rescuers, begin 15:2
IF they are UNDER PUBERTY and the arrest is witnessed, GET HELP FIRST
then return to the child and begin with compressions. Provide 2 minutes of
CPR and re-check for a pulse.
When you see a child collapse, (WITNESSED) you know their last breath and
last heartbeat was just now. Their blood oxygen level should be pretty high. So
get help first. If there are others around, send someone to get help and get
and AED.
If you find a child who has collapsed and it was unwitnessed, you have no idea
if their blood oxygen level is adequate, so provide 2 minutes of CPR first to get
their blood oxygen level back up, and then leave the child to go get help. If
there are others around, send someone to get help and get and AED.
IF the arrest is NOT witnessed, Begin 2 minutes of CPR, go get help and an
AED and return to the child. Begin cycles of 30 compressions and 2 breaths if
you are alone. Check a pulse every 2 minutes.
If there are two rescuers and the child is under puberty, begin cycles of 15
compressions and 2 breaths. Check a pulse every 10 cycles or 2 minutes.
Rescue Breathing Rate During CPR With an Advanced Airway
For infants and children with a pulse but absent or inadequate respiratory
effort give 1 breath every 2 to 3 seconds (20 to 30 breaths/min). It is the same
rate if an advanced airway is in place
CHOKING
For adults and older children, begin with 5 back slaps and then wrap your
hands around the victim's waist and begin 5 abdominal thrusts until the
victim becomes unresponsive or until the foreign object is removed.
For an infant, lay them over your forearm supporting the infant's head and
neck and begin 5 back slaps (Be sure to cradle the infant face down with head
lower than the rest of the body).
Turn the infant over and begin 5 chest
thrusts 2025 changed this to using the palm of your hand to give the chest
thrusts. (Do this with the palm of your hand, just as you would chest
compressions). Continue with 5 back slaps and 5 chest compressions until the
object is removed or the infant becomes unconscious.
Once an adult, child or infant becomes unresponsive, do not continue to treat
them as a chocking victim. Lay them on a hard flat surface and begin Basic
Life Support. Start by tapping and shouting "Hey, Are you Ok ?" Assess
breathing, if no breathing or only gasping, activate emergency response and
get an AED. Begin chest compressions. Before giving breaths, look in the
mouth for the obstructing object. If you can see the object, try to remove it.
Do not perform a blind finger sweep.
Attempt to give 2 rescue breaths. If the chest does not rise, reposition the
airway and attempt again. If the chest does not rise, begin chest
compressions. Between chest compressions and rescue breath attempts, it is
hoped that the back and forth motions will move the object one way or the
other. Continue as long as you can and just know, that you cannot continue
CPR forever. There may be a time when it is just not humanly possible to
continue for hours and hours, nor would you want to continue CPR on
someone for that length of time.
The chances of successfully reviving someone without significant brain
damage after an extended amount of time are very slim.
In some circumstances of extreme cold weather or drowning in cold water,
CPR should be continued until the person arrives at the hospital. The cold will
slow their oxygen demand and slow their heart rate. Depending on the
circumstances there is a fair chance of a good outcome if the person is cold.
So continue CPR as long as you can. But, remember, you are only human. You
cannot expect to perform CPR for hours on end. There will be a time that you
cannot humanly continue, and it is ok to stop CPR.
Control of Life-Threatening Bleeding
A manufactured tourniquet should be used as first-line therapy for
life-threatening extremity bleeding and should be placed as soon as possible
after the injury.
If a manufactured tourniquet is not immediately available or if a properly
applied manufactured tourniquet fails to stop bleeding, direct manual
pressure, with the use of a hemostatic dressing if available, should be used to
treat life-threatening extremity bleeding.
For individuals with life-threatening external bleeding, direct manual pressure
should be applied to achieve initial bleeding cessation for wounds not
amenable to a manufactured tourniquet or when a manufactured tourniquet
is not immediately available.
I hope you learned a lot from this extra information, please share the information with your friends and family!
The BLS Course focuses on preparing students to perform CPR skills. CPR is a life saving procedure for a victim who has signs of cardiac arrest (unresponsive, no normal breathing, and no pulse). Components of CPR are chest compressions and breaths.
High-quality CPR improves a victim's chances of survival. Study and practice the characteristics of high-quality CPR so that you can perform each skill effectively.
High-Quality CPR
Start compressions within 10 seconds of recognition of cardiac arrest.
Push hard, push fast: Compress at a rate of 1-- to 120/min with a depth of
-At least 2 inches or 5 centimeters for adults
-At least one third the depth of the chest, about 2 inches or 5 cm for children
At least one third the depth of the chest, about 1 1/2 inches or 4 cm for infants
Allow complete chest recoil after each compression.
Minimize interruptions in compressions (try to limit interruptions to less than 10 seconds).
Give effective breaths that make the chest rise.
Avoid excessive ventilation.
Chest Compression Depth
Chest compressions are more often too shallow than too deep. However, research suggests that compression depth greater than 2.4 inches (6cm) in adults may cause injuries. If you have a CPR quality feedback device, it is optimal to target your compression depth from 2 to 2.4 inches (5 to 6 cm).
The BLS techniques and sequences presented during the course offer 1 approach to a resuscitation attempt. Every situation is unique. Your response will be determined by
-Available emergency equipment
-Availability of trained rescuers
-Level of training expertise
-Local protocols
Personal Protective Equipment
Personal protective equipment (PPE) is equipment worn to help protect the rescuer from health or safety risks. PPE will vary based on situations and protocols. It can include a combination of items such as
-Medical gloves
-Eye protection
-Full body coverage
-High-visibility clothing
-Safety footwear
-Safety helmets
Always consult with your local health authority or regulatory body on specific PPE protocols relevant to your role.
Life is Why
High-Quality CPR is Why
Early recognition and CPR are crucial for survival from cardiac arrest. Be learning high-quality CPR, you'll have the ability to improve patient outcomes and save more lives.
The Chain of Survival
At the end of this part, you will be able to
-Describe the importance of high-quality CPR and its impact on survival
-Describe all of the steps of the Chain of Survival
-Apply the BLS concepts of the Chain of Survival
Adult Chain of Survival
The AHA has adopted, supported, and helped develop the concept of emergency cardiovascular care (ECC) systems for many years. The term Chain of Survival provides a useful metaphor for the elements of the ECC systems-of=care concept.
Cardiac arrest can happen anywhere - on the street, at home, or in a hospital emergency department, intensive care unit (ICU) or inpatient bed. The system of care is different depending on whether the patient has an arrest inside or outside of the hospital.
The 2 distinct adult Chains of Survival which reflect the setting as well as the availability of rescuers and resources are:
-In-hospital cardiac arrest (IHCA)
-Out-Of-Hospital cardiac arrest (OHCA)
Chain of Survival for an In-Hospital Cardiac Arrest
For adult patients who are in the hospital, cardiac arrest usually happens as a result of serious respiratory or circulatory conditions that get worse. Many of these arrests can be predicted and prevented by careful observation, prevention, and early treatment of prearrest conditions. Once a primary provider recognizes cardiac arrest, immediate activation of the resuscitation team, early high-quality CPR, and rapid defibrillation are essential. Patients depend on the smooth interaction of the institution's various departments and services and on a multidisciplinary team of professional providers, including physicians, nurses, respiratory therapists, and others.
After return of spontaneous circulation (ROSC), all cardiac arrest victims receive post-cardiac arrest care. This level of care is provided by a team of multidisciplinary specialists and may occur in the cardiac catheterization suite and/or ICU. A cardiac catheterization suite or laboratory (sometimes referred to as a "cath lab") is a group of procedure rooms in a hospital or clinic where specialized equipment is used to evaluate the heart and the blood vessels around the heart and in the lungs. A cardiac catheterization procedure involves insertion of a catheter through an artery or vein into the heart to study the heart and its surrounding structures and function. Measurements are made through the catheter, and contrast material may be used to create images that will help identify problems. During the procedure, specialized catheter can be used to fix some cardiac problems (such as opening a blocked artery).
The links in the Chain of Survival for an adult who has a cardiac arrest in the hospital are
-Surveillance, prevention, and treatment of prearrest conditions
-Immediate recognition of cardiac arrest and activation of the emergency response system
-Early CPR with an emphasis on chest compressions
-Rapid defibrillation
-Multidisciplinary post-cardiac arrest care
Chain of Survival for an Out-Of-Hospital Cardiac Arrest
Most out-of-hospital adult cardiac arrests happen unexpectedly and result from underlying cardiac problems. Successful outcome depends on early bystander CPR and rapid defibrillation in the first few minutes after the arrest. Organized community programs that preparre the lay public to respond quickly to a cardiac arrest are critical to improving outcome from OHCA.
Lay rescuers are expected to recognize the victim's distress, call for help, start CPR, and initiate public-access defibrillation until EMS arrives. EMS providers then take over resuscitation efforts. Advanced care, such as administration of medications, may be provided. EMS providers transport the cardiac arrest victim to an emergency department or cardiac catheterization suite. Follow-up care by a team of multidisciplinary specialists continues in the ICU.
The links in the Chain of Survival for an adult who has a cardiac arrest outside the hospital are
-Immediate recognition of cardiac arrest and activation of the emergency response system
- Early CPR with an emphasis on chest compressions
-Rapid defibrillation with an AED
-Effective advanced life support (including rapid stabilization and transport to post-cardiac arrest care)
-Multidisciplinary post-cardiac arrest care
Pediatric Chain of Survival
In adults, cardiac arrest is often sudden and results from a cardiac cause. In children, cardiac arrest is often secondary to respiratory failure and shock. Identifying children with these problems is essential to reduce the likelihood of pediatric cardiac arrest and maximize survival and recovery. Therefore, a prevention link is added in the pediatric Chain of Survival
-Prevention of arrest
-Early high-quality bystander CPR
-Rapid activation of the emergency response system
-Effective advanced life support (including rapid stabilization and transport to post cardiac arrest care)
-Integrated post-cardiac arrest care
Cardiac Arrest or Heart Attack?
People often use the terms cardiac arrest and heart attack interchangeably, but they are not the same.
Sudden cardiac arrest occurs when the heart develops an abnormal rhythm and can't pump blood
A heart attack occurs when blood flow to part of the heart muscle is blocked.
High-Performance Rescue Teams
Coordinated efforts by several rescuers during CPR may increase chances for a successful resuscitation. High performance teams divide tasks among team members during a resuscitation attempt. As a team member, you will want to perform high-quality CPR skills to make your maximum contribution to each resuscitation team effort.
Main Components of CPR
CPR consists of these main components
-Chest Compressions
-Airway
-Breathing
Adult 1 -Rescuer BLS Sequence
IF the rescuer is alone and encounters an unresponsive adult, follow these steps
Step 1 - Verify that the scene is safe for you and the victim. You do not want to become a victim yourself
Step 2 - Check for responsiveness. Tap the victim's shoulder and shout. "Are you ok?"
Step 3 - If the victim is not responsive, shout for nearby help
Step 4 - Activate the emergency response system as appropriate in your setting. Depending on your work situation, call 9-1-1 from your phone, mobilize the code team, or notify advanced life support.
Step 5 - If you are alone, get the AED/defibrillator and emergency equipment. If someone else is available, send that person to get it.
Next, assess the victim for normal breathing and a pulse. This will help you determine appropriate actions.
To minimize delay in starting CPR, you may assess breathing at the same time as you check the pulse. This should take no more than 10 seconds.
Breathing
To check for breathing, scan the victim's chest for rise and fall for no more than 10 seconds.
-If the victim is breathing, monitor the victim until additional help arrives.
-If the victim is not breathing or is only gasping, this is not considered normal breathing and is a sign of cardiac arrest.
Agonal Gasps
Agonal gasps are not normal breathing. Agonal gasps may be present in the first minutes after sudden cardiac arrest.
A person who gasps usually looks like hi is drawing air in very quickly. The mouth may be open and the jaw, head, or neck may move with gasps. Gasps may appear forceful or weak. Some time may pass between gasps because they usually happen at a slow rate. The gasp may sound like a snort, snore, or groan. Gasping is not normal breathing. It is a sign of cardiac arrest.
Check Pulse
To perform a pulse chick in an adult, palpate a carotid pulse
First, locate the trachea, on the side of the neck closest to you. Slide these 2 or 3 fingers into the groove between the trachea and the muscles at the side of the neck, where you can feel the carotid pulse. Feel for a pulse for at least 5 seconds, but not more than 10.
IF you do not definitely feel a pulse within 1- seconds, begin high-quality CPR, starting with chest compressions. In all scenarios, by the time cardiac arrest is identified, the emergency response system or backup must be activated, and someone must be sent to retrieve the AED and emergency equipment.
If the victim is not breathing normally or is only gasping and has no pulse, immediately begin high-quality CPR, starting with chest compressions. Remove or move the clothing covering the victim's chest so that you can locate appropriate hand placement for compressions. This will also allow placement of the AED pads when the AED arrives.
After 30 compressions have been performed, use the head tilt, chin lift and give 2 rescue breaths while watching for chest rise and immediately resume chest compressions. Perform 30 compressions and 2 breaths for five cycles and recheck for a pulse. If there is still no pulse, resume chest compressions and breaths until help arrives, or until you are physically not able to continue. No one expects you to be able to continue CPR forever. You will eventually become exhausted and unable to continue.
Defibrillation
Attempt Defibrillation Use the AED as soon as it is available, and follow the prompts
External Defibrillator for Adults and Children 8 Years of Age and Older
Resume High-Quality CPR
Immediately resume high-quality CPR, starting with chest compressions, when advised by the AED. Continue to provide CPR, and follow the AED prompts until advanced life support is available.
Importance of Chest Compressions
Each time you stop chest compressions, the blood flow to the heart and brain decreases significantly. Once you resume compressions, it takes several compressions to increase blood flow to the heart and brain back to the levels present before the interruption. Thus, the more often chest compressions are interrupted and the longer the interruptions are, the lower the blood supply to the heart and brain is.
High-Quality Chest Compressions
If the victim is not breathing normally or is only gasping and has no pulse, begin CPR, starting with chest compressions.
Single rescuers should use the compression-to-ventilation ratio of 30 compressions to 2 breaths when giving CPR to victims of any age.
When you give chest compressions, it is important to
Caution
Do Not Move the Victim During Compressions
Do not move the victim while CPR is in progress unless the victim is in a dangerous environment (such as a burning building) or if you believe you cannot perform CPR effectively in the victim's present position or location.
When help arrives, the resuscitation team, based on local protocol, may choose to continue CPR at the scene or transport the victim to an appropriate facility while continuing rescue efforts.
Foundational Facts
The Importance of a Firm Surface
Compressions pump the blood in the heart to the rest of the body. To make compressions as effective as possible, place the victim on a firm surface, such as the floor or a backboard. If the victim is on a soft surface, such as a mattress, the force used to compress the chest will simply push the body into the soft surface. A firm surface allows compression of the chest and heart to create blood flow.
Chest Compression Technique
Compressions in an adult:
Position yourself at the victim's side.
Make sure the victim is lying face up. on a firm flat surface. If the victim is lying face down, carefully roll him to a face up position.
Position your hands and body to perform chest compressions:
• Put the heel of one hand in the center, of the victim's chest, on the lower half of the breastbone (sternum).
• Put the heel of your other hand on top of the first hand.
• Straighten your arms and position your shoulders directly over your hands
Give chest compressions at a rate of 100 to 120/min.
Press down at least 2 inches (5 cm) with each compression (this requires her Work). For each chest compression, make sure you push straight down on the victim's breastbone.
At the end of each compression, make sure you allow the chest to recoil complete, Minimize interruptions of chest compressions (you will learn to combine compressions with ventilation next).
Chest Recoil
Chest recoil allows blood to flow into the heart. Incomplete chest recoil reduces the fling of the heart between compressions and reduces the blood flow created by chest compressions. Chest compression and chest recoil/relaxation times should be about equal.